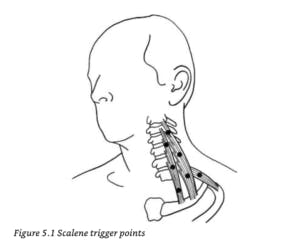
In the context of physical therapy, massage therapy, orthopedics and other clinical settings, you may have heard the term Trigger Point being used to explain the cause of some of your symptoms. Today, we are going to focus on what these trigger points are, how they might contribute to some of the symptoms you may be feeling, and describe in detail a Scalenes trigger point release technique. Why do we care specifically about the Scalenes Muscles? Your scalenes, as we will describe below, are frequent culprits when it comes to neck, shoulder, scapula and arm pain. In addition, they are often affected by anxiety, stress and poor posture, all of which we are dealing with more than ever during these challenging times!
For additional information regarding trigger points, we highly recommend Clair and Amber Davies’s The Trigger Point Therapy Workbook: Your Self-Treatment Guide for Pain Relief. In addition to more information on the scalenes trigger point release, there you will find excellent descriptions of common trigger points, referred pain patterns, and self-treatment guides. Unless otherwise specified, most descriptions and images below come from this very helpful resource.
What are “Trigger Points”?
Clinically speaking, the term Trigger Point refers to any painful point that develops within muscle tissue. They can be present within any muscle, and tend to develop after long-term or inappropriate stress is placed on that muscle (see below for examples of stressors). Trigger points can be thought of as “active” or “latent”. Fernández de Las Peñas et al (2017) conducted an international consensus review to establish clinically relevant definitions for “active” versus “latent” points, and came up with the following distinctions:
- Active Trigger Point: causes a clinical pain complaint
- Always tender, and may prevent full muscle lengthening (make your muscles feel tight)
- Cause muscle weakness
- When compressed, refers a patient-recognized pain, and/or motor phenomenon (i.e. twitching)
- When stimulated may cause a local twitch response of muscle fibers compressed within the patient’s pain tolerance
- Latent Trigger Point: clinically inactive with respect to spontaneous pain
- Painful only when palpated (meaning “touched” or “pressed on”)
- May have all the other clinical characteristics of active TPs
- Always has a taut band that increases muscle tension and restricts range of motion
What are your Scalenes?
The Scalenes are a muscle group that help stabilize, flex (bend forward), laterally flex (tilt the head to the side), and rotate the neck. They also help raise your upper two ribs when you inhale, meaning they are working every time you breathe. However, they work HARDEST during labored breathing, i.e. during vigorous activity, coughing, sneezing, or during periods of anxiety (hence, why they may be more bothersome to some people at this time!)
Where are your Scalenes?

- Anterior Scalene: the front-most scalene muscle, lies between the SCM (sternocleidomastoid) and the neck vertebrae and is almost completely hidden
- Middle Scalene: is behind the anterior scalene, more on the side of the neck, with its lower half free of the SCM
- Posterior Scalene: almost horizontal, behind the middle scalene in a triangular groove just above the collarbone (clavicle) and below the front edge of the upper trapezius (the bulkier muscles that help you shrug your shoulders)
What do Trigger Points in the Scalenes Feel Like?
As described above, trigger points themselves can create a number of different sensations. If you have trigger points throughout your Scalenes that are more active, you may feel some pain or symptoms throughout your shoulder blade/scapula, shoulder joint, side of your arm, forearm and fingers, up to your neck, into your chest, or in a combination of some or all of these locations.

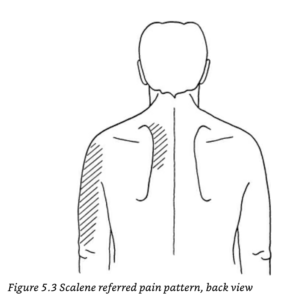
Trigger points in your Scalenes, when pressed on, can produce particularly “strange” sensation, sometimes described as “nervey”, “weird”, “burning”
What causes the development of trigger points within the Scalenes?
1. Not-So-Great Breathing
Improper breathing patterns such as chest breathing (breathing so that your chest rises with every breath) or nervous hyperventilation will overtax the scalene muscles. Who is prone to these types of breathing patterns?
- Those experiencing emotional tension, anxiousness or stress (for example, anyone who might currently find themselves in either social isolation OR working in close proximity with ill individuals…).
- Individuals with chronic respiratory conditions such as asthma or emphysema that make breathing more labored.
- Individuals with new or worsening respiratory conditions such as pneumonia, bronchitis, allergies, or a common cold that result in constant coughing.
2. Improper Body Positioning
- Working for long hours with the arms out in front of the body can be very stressful for your Scalenes, including working at your computer. Pulling, lifting, and carrying heavy loads can also cause stress, including rearranging heavy furniture or an intense day of spring cleaning.
- Carrying a heavy grocery bags or backpacks.
- Maintaining improper posture – your Scalenes are largely responsible for managing the weight of the head, which is quite heavy! Any posture you assume where your head is not supported, or that puts your head in front of or behind your upright torso creates an imbalance and puts an additional burden on them.
So, what can you do at home to address symptoms that might be caused by Scalenes Trigger Points?
First, try to adjust some of the habits that might be creating them in the first place:
- Focus on proper diaphragmatic breathing. Diaphragmatic breathing refers to breathing so that your belly rises with every breath instead of your chest or shoulders. This type of breathing is often used during meditation and relaxation sessions and can help with mental as well as physical stress. This video from Mass General Hospital helps demonstrate good diaphragmatic breathing technique.
- Focus on maintaining good, neutral posture in sitting, standing and sleeping positions. To do this while sitting and standing, you can think about “reaching” your head straight up towards the ceiling, almost as if it is being pulled up by an invisible thread – feel yourself “creating space” in between each vertebrae as you elongate your spine. While lying down, focus on giving your head and legs proper support so that your spine, head and hips remain as aligned as possible. For some quick tips, you can watch this video, or feel free to reach out to a Physical Therapist for a more targeted consultation!
Next, try a Scalenes Trigger Point Release technique!
STOP – CONTRAINDICATIONS: Before moving onto the technique, it is important for us to make you aware of some of the reasons you should not continue. We always recommend consulting with a healthcare professional before attempting any self-release technique if there is a possibility of fracture, nerve damage, cardiovascular disease or blood vessel compromise in the area you plan to massage. If you have been through a recent physical trauma or accident, or have experienced any of the following symptoms, do not attempt this technique, and seek medical attention:
- Dizziness and/or unsteadiness
- Diplopia (double vision or visual field loss)
- Dysarthria/dysphasia (difficulty speaking or finding the right words)
- Dysphagia (difficulty swallowing or sudden hoarseness of voice)
- Drop attacks (sudden collapse without loss of consciousness)
- Nystagmus (uncontrolled sideways movement of the eyes)
- Nausea or vomiting
- Numbness or paraesthesia (altered light touch sensation), particularly around the mouth
Scalenes Self-Trigger Point Release Technique
In order to fully address any pain or symptoms that might be coming from scalenes trigger points, it is important to move as methodically as possible through all 3 major branches of the scalenes: Anterior, Middle & Posterior. Below we have described how to find each branch and perform your self-release technique.
General Guidelines:
- Clip or file your fingernails prior to starting this technique – long nails are not your friend when digging into the side of your neck!
- Use short strokes in either a straight line, no more than half an inch long, or in small circular strokes, both performed with 1-2 fingers. For hard to reach places, feel free to use a lacrosse ball or tennis ball (this applies more to techniques being used for muscles of the back, hips and legs that are bulkier and/or harder to reach with your hands).
- Make sure you focus on performing strokes at multiple points throughout each muscle, instead of focusing on just one point over and over.
- Focus on performing 10-12 strokes per tender spot, 3-6 times per day
- When pressing on a trigger point, you should feel no more than a 4 or 5 on a scale of 1-10 pain, 1 being very minimal pain, 10 being “emergency room level pain” or “the worst pain you have ever felt”
- If you can feel your pulse under your fingers, do not press down! You have found your carotid or subclavian pulses, which are great for helping you know you are alive, but not great for finding places to press down hard.
- Don’t be too concerned about getting the massage exactly right. As long as you are aware of and adhere to the contraindications listed above, pay attention to your symptoms and pain level, avoid pressing on pulse points, and check-in with how you are feeling before and after your self-treatment, it is highly unlikely that you will cause yourself any harm! That being said, if you feel at all uncomfortable with performing this technique, or have additional questions you’d like answered before trying it out, feel free to reach out to a Physical Therapist for help!
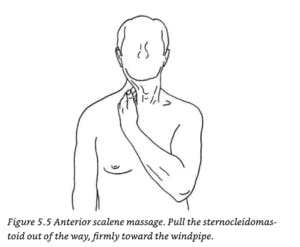
Anterior Scalene
- Get your fingers between the neck vertebrae and the sternocleidomastoid (SCM) – the SCM will feel like a “rope of muscle” that runs from your ear down to your sternum.
- Grip the SCM between the fingers and thumb, of the opposite hand, as if you were going to massage it.
- Let go with your thumb and with your fingers pull the entire SCM about two inches toward the windpipe.
- With your fingers, press directly back – this should pin the anterior scalene against your vertebral column in order to create nice pressure underneath your fingertips.
Middle Scalene
- Repeat steps 1-3 above.
- Starting just below your ear, press into the side of your neck. You may feel some “bony knobs” under your fingertips – these are the transverse processes (or sides) of your vertebrae. You want to make sure that you are in front of these knobs. Otherwise, you are likely massaging muscles in the back of your neck (which, to be fair, is not bad at all, but just not what you are looking to do right now).
- You can confirm that you are in the right position by quickly taking a few short, repeated breaths – you should feel the muscle twitching below your fingers.
- On the side of the neck here, use the same stroke you used for the anterior scalene.
- Follow this muscle all the way from just below the ear down to the middle of the collarbone.

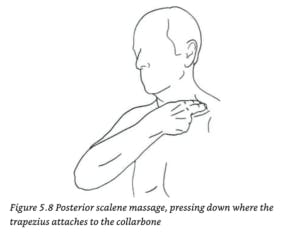
Posterior Scalene
- Push your middle finger under the front edge of the trapezius muscle near where it attaches to the collarbone.
- Press downward and drag your finger an inch or so toward your neck in a short, straight line parallel to your collarbone. In this case, the bone you might feel under your fingers is your first rib.
Feel free to try this Scalenes trigger point release out at any point throughout your day. If you have any questions or comments, certainly feel free to reach out! We are open for new visits and telehealth sessions to address your needs throughout this time. Thanks for reading!
References:
Davies, Clair. The Trigger Point Therapy Workbook: Your Self-Treatment Guide for Pain Relief (A New Harbinger Self-Help Workbook) (p. 101). New Harbinger Publications. Kindle Edition.
Fernaindez De Las Penas, C., & Dommerholt, J. (2017). International Consensus on Diagnostic Criteria and Clinical Considerations of Myofascial Trigger Points: A Delphi Study. Pain Medicine, 19(1), 142-150. doi:10.1093/pm/pnx207
Also, feel free to read up on more helpful techniques at home, such as Telehealth for Brooklyn-based Physical Therapy and Increasing Shoulder Range of Motion.
.png?auto=format&auto=compress&h=150)