The Schroth Method for scoliosis utilizes a three dimensional approach to elongate the trunk and correct imbalances of the spine. The goal is to develop the inner muscles of the rib cage in order to change the shape of the upper trunk and to correct any spinal abnormalities.
Developed by Katharina Schroth
The Schroth Method was originally developed by Katharina Schroth in Germany. The method uses customized exercises to return the body’s posture to a more natural position. It is standard treatment for scoliosis in many European countries, and is gaining trust and popularity in the United States.
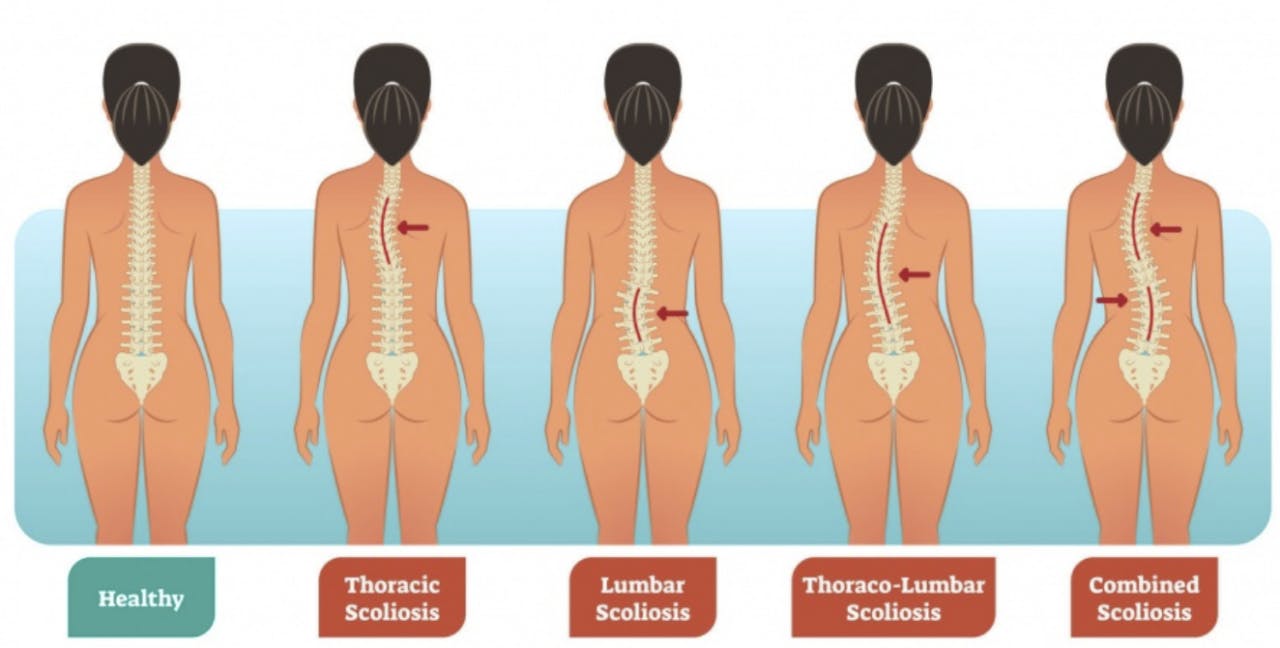
Scoliosis Symptoms
Symptoms of Scoliosis vary. Pain does not always accompany scoliosis. As a result, scoliosis can present in a variety ways such as abnormal trunk lean, uneven rib cage/shoulders or even back pain. If you suspect scoliosis contact your primary care provider. Prior to Schroth treatment, an x-ray is needed as scoliosis can present differently externally due to overlying musculature and does not give us the full picture. So, knowing the bony anatomy allows us to monitor your progress and tailor your treatment to your specific curvature.
Treatment at Park Sports PT
Getting treatment at Park Sports PT means you are working with certified therapists trained in the Schroth Method. They are partners in your health and wellness. Your therapist will create a personalized plan just for you and your specific condition. Our treatment approach can treat scoliosis patients of all ages. It can also can be utilized to treat in all stages of scoliosis, including after surgery.
Throughout treatment, we look closely at the three-dimensional curve in the spine. We teach patients very specific ways to correct that curve or scoliosis posture. Once patients have recognized their corrected posture, we teach them breathing and muscle activation techniques to hold that correction. Essentially, we help train the motor neurons to sense when they’re in a corrected posture versus when they’re in their scoliosis posture.
The Schroth Method takes a lot of repetition and commitment from the patient to learn these techniques. That’s why home exercises are also recommend at least five days a week for a half hour each time.
Trial results show improved patient outcomes
Several trials have found that physical therapy scoliosis-specific exercises lead to improved patient outcomes. This includes less pain and improved muscular strength, muscular endurance and self-image. In one study, spinal deformity improved in 69 percent of patients who completed Schroth exercises. This compared to only 6 percent in patients who did not complete their exercises. The Schroth Method at Park Sports PT works.
Your Park Sports PT team will create a personalized plan and will help prepare you to work on your strength and posture at home. The result is long term care and a stronger and healthier body.
Contact Us
If you or your child has any symptoms or have visited your primary care provider and are looking for treatment, contact us today to learn more. We are here to help.
.png?auto=format&auto=compress&h=150)