Are you feeling back pain from cycling? Given how hard your legs work when you’re on your bike, it’s natural to assume that your knees would be most vulnerable to a cycling injury. However, research suggests that the biggest culprit is not knee pain but lower back pain!
Let’s discuss why cyclists are suffering from back pain and how you might prevent it.
How to Prevent Back Pain From Cycling
You might be surprised at the number of people who are afflicted with back pain from cycling, given that it is a low-impact sport and is often recommended for those who suffer from back pain. Why is lower back pain so common among cyclists? It might be your bike setup.
Start With Correct Bike Set-Up
Though lower back pain often occurs because of muscle weakness or improper movement as a result of fatigue, one thing we recommend is to assess your bike fit, too, as this can also be a contributing factor. You want to choose a bike frame with the proper geometry to ensure the correct riding position, which can help minimize the pain on not only your lower back but your knees, shoulders, and even your neck.
When you’ve found a frame that suits you, the next step is to set up on it correctly. There are a few key elements to look at. First, the saddle height should be positioned so that when the pedal is at the bottom of the stroke, and the ball of your foot is on the pedal, your knees are slightly bent. Hips shouldn’t move sideways during crank rotation, and you shouldn’t have to stretch at the bottom of the pedal stroke.
Saddle angle is also critical. It should be in a horizontal position, parallel with the floor (sometimes a very slight downwards tilt can be helpful for those who experience pressure in the perineum area).
Handlebars should be adjusted as well. You should adjust them so that you don’t have to stretch to reach them, but they shouldn’t be too close to your body either. You want your arm position to be comfortable when you reach for them in an upright position, and your elbows should be slightly bent.
Work Your Core
A significant factor that plays into back pain is muscle fatigue and the resulting poor posture to accommodate. Some studies suggest that when cyclists are pedaling to exhaustion, their hamstrings and calf muscles became tired, resulting in undesirable changes in muscle movement patterns. The degree to which you bend forward in the lumbar region and how far your knees are splayed out affects your back. Basically, the more tired you become in your legs, the worse your spinal posture gets.
The evidence points to the fact that to avoid muscle fatigue and strengthen your lower back to prevent pain due to impaired movement patterns, you must work on your core. Your core is your foundation, so if your core is weak, then your lower back muscles will likely try to compensate, leading to overworking, stress on the joints and ligaments within your spine, stiffness, and pain.
A certified therapist like those at Park Sports Physical Therapy in Brooklyn can give you some outpatient therapy and equip you with a plan of safe exercises to practice based on your functional strength and pain symptoms.
Stretch Before and After Riding
Several things can lead to lower back pain. Tight hamstrings are common for cyclists as they pull the pelvis down and cause the lower back to curve more than it should. Tight hip flexors, quadriceps, piriformis, and other muscles can lead to back pain as well. The more flexible you are, the more efficient your cycling will be, and the less likely you’ll experience pain from improper positioning.
There are lots of stretches you should do before and after you ride. Reach out to our team for a complete list of great stretches for cycling. Yoga and pilates, in general, will help you stay limber.
Contact Park Sports PT If You’re Suffering With Back Pain From Cycling
Lower back pain in cyclists is a very common injury. Some studies suggest that more than half of all cyclists have experienced lower back pain in this year alone. The two main reasons why back pain from cycling happens are incorrect bike geometry or muscular insufficiency, and sometimes both! If you’re a cyclist or are planning to spend more time on your bike this summer, make sure that your bike is properly fitted. Bike shops can be a huge help here.
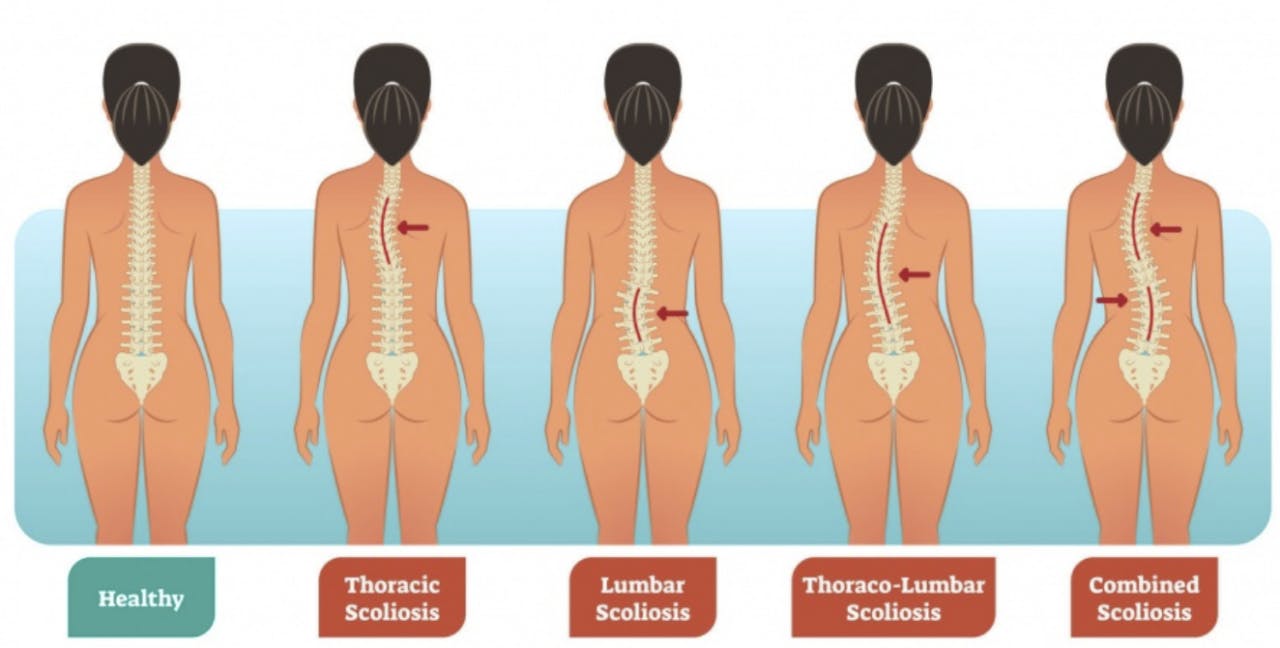
Muscular insufficiency can be addressed in physical therapy. We know that sitting in the saddle for a long time causes the muscles in your calves, hamstrings, and behind your back to naturally shorten. This position changes the length-tension ratio of the muscles and creates multiple issues that could lead to pain. Additionally, prolonged pedaling causes fatigue, which leads to undesirable muscle movement patterns in the legs and spine. It affects your bike by altering the spinal posture. Physical therapists usually associate excessive lumbar spine flexion with lower back pain in cyclists. Excessive lumbar spine flexion is associated with the reduced activity of a key back muscle, multifidus, a stabilizing muscle located in the deep layer of your back.
At Park Sports, we’ll build you a comprehensive lower extremity stretching program and a core stabilization program for cyclists suffering from back pain. We think that back pain from cycling can be avoided, it just comes down to understanding the basic principles of biking mechanics and building up your core so that you can get back to the things you love, pain-free!
When you need us, the physical therapists at Park Sports know all the ins and outs of the mechanical aspect of cycling. We are passionate about sports and athletics, and some of our team members are advanced-level multi-sport athletes that include cycling. Our office is located at Prospect Park, a major cycling venue in Brooklyn. Give us a call to schedule a consultation or a meeting; we would love to help!
.png?auto=format&auto=compress&h=150)